Overview
An Explanation of Benefits (EOB) is not a bill. It is a statement sent to members after a provider submits a claim. It outlines how the claim was processed, including:
- The total amount billed by the provider
- The amount covered by the insurance plan
- Discounts applied through the network or legal protections
- The remaining amount the member may owe
- Progress toward the plan’s deductible and out-of-pocket maximums
Key Sections of the EOB
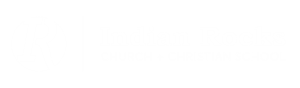
Member/Patient Information
Identifies who received care, including the member’s ID, relationship to the subscriber, group name, and group number.
Claim Summary
Provides a high-level overview of the services received, the amount billed by the provider, and the total amount the member is responsible for.
Plan Balances
Displays current progress toward both individual and family deductibles and out-of-pocket limits. Includes separate breakdowns for in-network and out-of-network services.
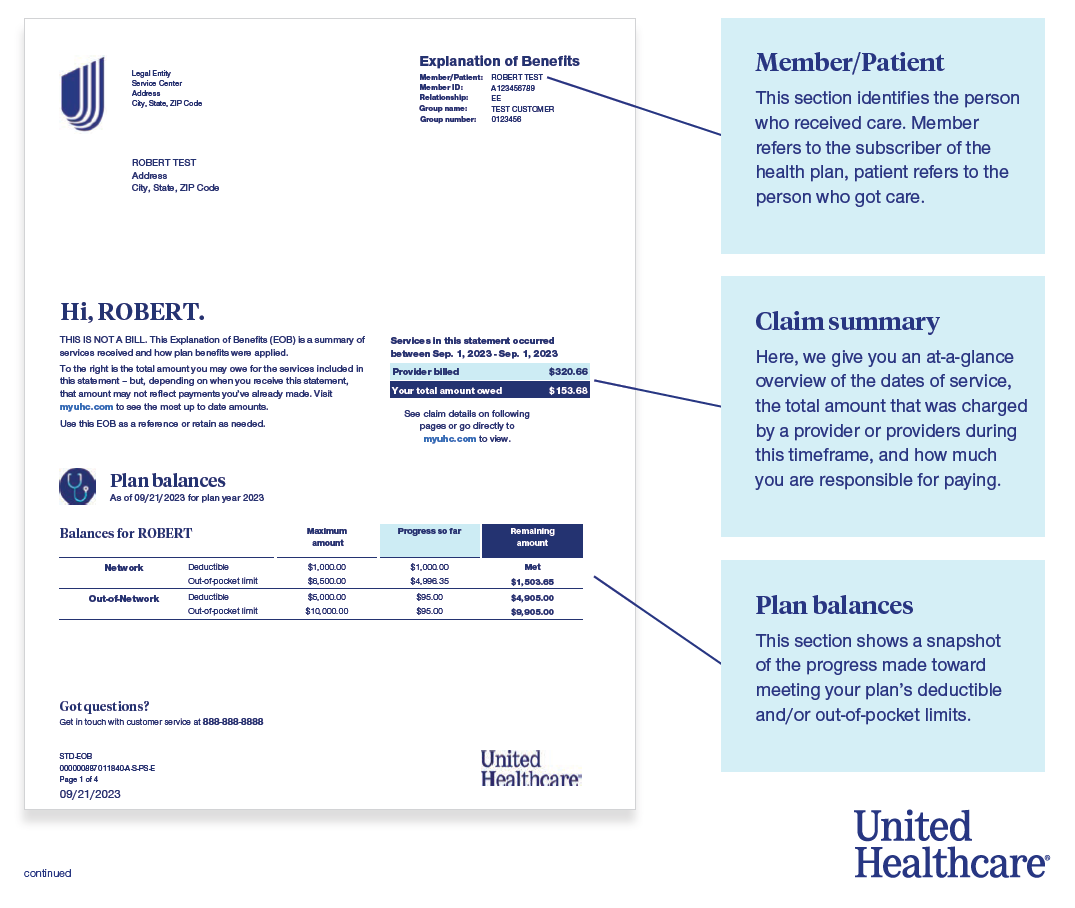
Claim Detail
Breaks down each service received, including:
- Provider billed amount
- Amount saved through discounts
- Plan allowed amount
- What the plan paid
- What was applied to deductible
- Member’s coinsurance or copay amounts
- Final amount owed by the member
Claim Processing Codes
Used to explain specific adjustments made during claims processing.
Examples:
- UG: Network discount applied; deductible not met
- 2Q: Adjustment due to multiple procedure payment policy
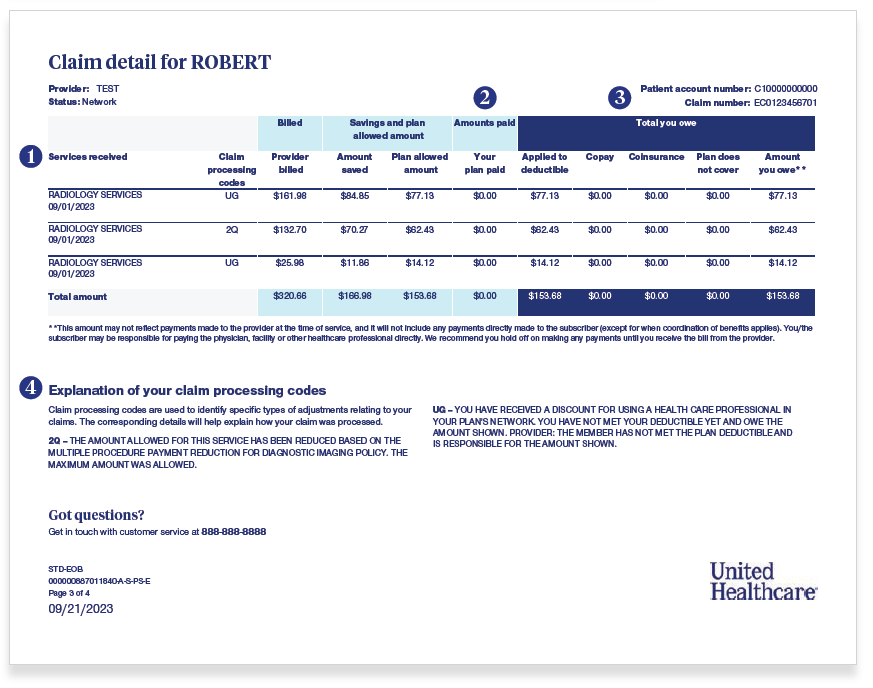

Definitions to Know
- Deductible: The amount the member must pay out of pocket before the plan starts covering costs.
- Amount You Owe: The portion the member is responsible for paying.
- Plan Does Not Cover: Any service or charge not covered under the member’s plan.
Member Reminders
- The EOB is not a bill. Members should wait for the actual bill from the provider before making payments.
- The amount shown as “You may owe” could be different if payment was made at the time of service or if the provider sends a separate bill later.
- Members can log into myuhc.com to view up-to-date claims status, payment details, and plan balances.
Need More Support?
We are here to help! If you have a claim or bill that you don’t understand or can’t resolve, contact Human Resources. We are here to help and can connect you with support at UnitedHealthcare directly to find a solution.